1. A young patient is diagnosed with torticollis. However, radiographs do not confirm a skeletal cause for the patient's head tilt and rotation. Nothing suggests a neoplastic origin for the disorder. What other tests/examinations should be performed:A. Gastroenterologic examination
B. Stretching exercises
C. Ophthalmologic examination
D. Laboratory tests
E. A and C
2. Which of the following can be the presenting symptoms of patients with cervical myelopathy?a. Gait disturbance
b. Clumsiness and loss of manual dexterity
c. Weakness in the lower extremities
d. Urinary incontinence
e. All the above
3. A unilateral decrease in the triceps reflex is most likely evidence of what clinical syndrome?a. C5 radiculopathy
b. C6 radiculopathy
c. C7 radiculopathy
d. Cervical myelopathy
e. None of the above
4. Which of the following physical findings is consistent with cervical myelopathy?a. A hyperactive knee-jerk
b. A positive jaw-jerk
c. Cog-wheel rigidity
d. Absent ankle reflexes
e. A positive axial manual traction test
5. Which of the following pathologic changes IS NOT seen in cervical spondylosis?a. Increased water in the nucleus pulposus
b. Loss of annular elasticity
c. Disk space narrowing
d. Disk protrusion
e. Osteophyte formation
6. In an otherwise healthy 57-year-old patient, which of the following represents the most pressing relative indication for surgical treatment?a. A history of chronic, severe axial neck pain
b. A large herniated disk on MRI of the neck
c. Cervical radiculopathy with neurologic findings
d. Cervical myelopathy
e. All the above require surgical treatment
7. What is the most common instability pattern seen in patients with rheumatoid arthritis of the cervical spine?a. Atlantoaxial instability
b. Basilar invagination
c. Subaxial instability
d. Mixed
e. No one pattern is most common
8. A 6-year-old boy has neck pain and stiffness following an upper respiratory tract infection. He presented with his head tilted to the right and turned to the left 3 weeks ago, but a soft cervical collar has not been beneficial. There is no known history of trauma. A computerized tomography scan shows rotatory subluxation of C1 on C2. The next step in the treatment of this child is:a. Observationb. Open reduction and C1-C2 fusion through an anterior approachc. In situ C1-C2 fusion posteriorlyd. Cervical tractione. Hard cervical collar9. If the C7 cervical spine nerve root is injured during a posterior decompression of the cervical spine, then sensation is lost in which of the following areas:a. The lateral aspect of the arm from the shoulder to the elbowb. The medial aspect of the arm from the shoulder to the elbowc. The lateral border of the forearm including the thumb d. The middle fingere. The medial border of the forearm including the little fingerAnswers:1. E. Acquired torticollis may have several etiologies including neurologic, traumatic, or inflammatory. Sandifer's syndrome is a term used for gastroesophageal reflux accompanied by torsion spasms of the neck. Ocular torticollis occurs in children with alignment disorders (strabismus) causing them to tilt their heads to avoid diplopia. Stretching exercises to relieve torticollis work well only in congenital cases and before patients reach 1 year of age.
2. e.
Any or all of the above may be seen in a patient with cervical myelopathy. Abnormality of gait, particularly a broad-based and shuffling gait, is the hallmark abnormality of cervical myelopathy, but any of the above can be seen.
3. cThe triceps reflex is innovated by C7, and a diminished triceps reflex would be seen in a C7 radiculopathy.
4. aCervical myelopathy results in upper motor neuron findings for spasticity including hyperreflexia of the lower extremities, up-going toes, and, depending on the level of the spinal cord compression, hyperactivity in the upper extremities.
5. aSpondylosis of the cervical (or lumbar) spine includes disk degeneration. The first and most striking finding in disk degeneration is a decrease in water content of the nucleus pulposus. All the other abnormalities are indeed seen in cervical and lumbar spondylosis.
6. dIn a relatively healthy, middle-aged patient, the presence of cervical myelopathy represents a fairly clear-cut indication for surgical treatment. The presence of chronic severe axial neck pain is usually treated nonoperatively. Patients with a herniated disk, even with evidence of radiculopathy, are usually treated nonoperatively, and that is certainly the first line of treatment in most cases.
7. aAll the above patterns of instability, including mixed patterns involving C1–C2, the occipitocervical junction, and the subaxial spine can be seen. Instability at C1–C2, however, is the most common pattern of instability seen.
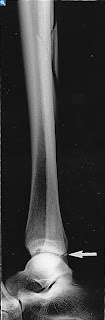
8. dThis child has torticollis as sequelae of an upper respiratory infection (Grisel syndrome) and rotatory subluxation (fixation) of C1 on C2. Other causes of torticollis include congenital muscular torticollis, neurogenic causes, Sandifer syndrome, Klippel-Feil syndrome, juvenile rheumatoid arthritis, and trauma. The common thread is that all of the etiologies appear to weaken, through inflammation or force, the supporting soft tissue structures of the atlantoaxial articulation. The diagnosis is made by dynamic CT scan.
Fielding classified atlantoaxial rotatory subluxation into 4 types:
- Type I is a simple rotatory displacement without an anterior shift, and is the most common type in children.
- Type II is rotatory fixation with anterior displacement >3 to 5 mm, and is associated with a deficiency of the transverse ligament and unilateral displacement of one lateral mass of the atlas.
- Type III rotatory fixation there is anterior displacement >5 mm with bilateral displacement of the lateral mass with one side displaced more than the other. This is caused by a deficiency of both the transverse ligament and secondary ligament.
- Type IV is rotatory fixation with posterior displacement where the dens allows posterior shift of one or both of the lateral masses, and one shifting more than the other.
Types III and IV are rare but have potential for catastrophe and should be recognized to promptly initiate treatment.
Children with rotatory fixation of <1>
9. d
The C7 cervical spine nerve root supplies sensation to the skin over the volar aspect of the middle finger.
- C5 — Lateral aspect of the arm from the shoulder to the elbow
- C6 — Lateral border of the forearm including the thumb
- C7 — Middle finger
- C8 — Medial border of the forearm including the little finger
- T1 — Medial aspect of the arm from the shoulder to the elbow